FALLS IN THE ELDERLY
THE NUMBERS & STATS
33%
of people over 65 have a fall each year.
50%
of people over 80 have a fall each year.


10%
of falls
result in a fracture

A hip fracture costs the NHS
£12,000...
+
£3,500 in social care
£3,500 in social care

Every 10 seconds in the UK, someone over 65 suffers a fall!

Every 10 seconds in the UK, someone over 65 suffers a fall!

Every HOUR someone over 65
DIES due to a hip fracture
33% of people over 60
who fracture their hip DIE within a year

Every HOUR someone over 65
DIES due to a hip fracture
33% of people over 60
who fracture their hip DIE within a year
Falls are the most common cause of death from injury in over 65s
COSTS
OF FALLS BY ELDERLY
Falls cost the NHS 2.3 billion a year

Falls cost the NHS 2.3 billion a year

Falls are the largest
cause of emergency hospital admissions
for older people
Hip fractures cost £6 Million / day
Hip fractures cost £6 Million / day
THE NUMBERS
FALLS AND REPERCUSSIONS

THE NUMBERS
FALLS AND REPERCUSSIONS

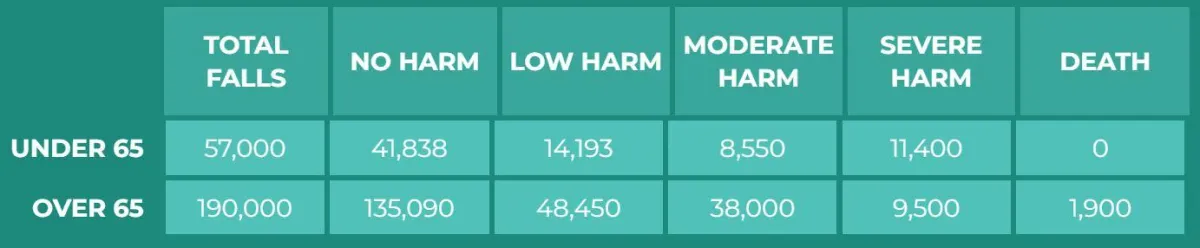
TOTAL FALLS
NO HARM
LOW HARM
MODERATE HARM
SEVERE HARM
DEATH
UNDER 65
57,000
41,838
14,193
8,550
11,400
0
OVER 65
190,000
135,090
48,450
38,000
9,500
1,900
Falls account for 40%
of nursing home admissions
Falls account for 25%
of all hospital admissions
Falls account for 40%
of nursing home admissions
Falls account for 25%
of all hospital admissions
40% of those who fall don't
return to independent living
...and 25% of those DIE
within a year
40% of those who fall don't
return to independent living
...and 25% of those DIE
within a year
RESULTS OF FALLS
What happens following a fall?
RESULTS OF FALLS
What happens following a fall?
Distress
Pain
Injury
Loss of confidence
Loss of independence
Mortality 😢
Distress
Pain
Injury
Loss of confidence
Loss of independence
Mortality 😢
HOWEVER...
...Anti-fall programs can prevent 55% of falls
If over 65s followed a program it would prevent 7,000
deaths (19 per day) just from hip fractures.
Falling is NOT an inevitable part of ageing.
With the right knowledge and support, older people
can stay active and prevent falling.

REASONS FOR FALLS
Balance problems
and muscle weakness

Poor vision
Balance problems
and muscle weakness

Poor vision
It could also be a long-term health condition, such as heart disease, dementia or low blood pressure (hypotension) which can lead to dizziness and a brief loss of consiousness.
Dizziness from some medications,
standing too quickly or dehydration
Foot problems

Dizziness from some medications,
standing too quickly or dehydration
Foot problems

Alcohol

Alcohol

WHAT CAN WE DO?
TO REDUCE THE CHANCES OF FALLING...

Immediately mopping up spillages.
Removing clutter, trailing wires and frayed carpet.
Using non-slip mats and rugs.
Using high-wattage light bulbs in lamps and torches, so you can see clearly.
Organising zour yome so that climbing, stretching and bending are kept to a minimum, and to avoid bumping into things.
Getting help to do things that you're unable to do safely.
Not walking on slippery floors in socks and tights.
Not wearing loose-fitting, trailing clothes that might trip you up.
Wearing well-fitting shoes that are in good condition and support the ankle.
Regular sight tests.
Moderate alcohol consumption - alcohol can reduce coordination and
exaggerate the effects of some medication. Alcohol can also speed up the effects of oesteoperosis.
Immediately mop up spillages.
Removing clutter, trailing wires and frayed carpet.
Using non-slip mats and rugs.
Using high-wattage light bulbs in lamps and torches, so you can see clearly.
Organising zour yome so that climbing, stretching and bending are kept to a minimum, and to avoid bumping into things.
Getting help to do things that you're unable to do safely.
Not walking on slippery floors in socks and tights.
Not wearing loose-fitting, trailing clothes that might trip you up.
Wearing well-fitting shoes that are in good condition and support the ankle.
Regular sight tests.
Moderate alcohol consumption - alcohol can reduce coordination and
exaggerate the effects of some medication. Alcohol can also speed up the effects of oesteoperosis.
INCREASE BALANCE
THROUGH EXERCISE

Exercise programs can cut falls by more than half (up to 55%)
Otago home exercise program

The NHS has produced strength and balance programs for the over 60s to do at home

Falls prevention programs designed around dancing in local communities
INCREASE PROTEIN IN DIET
Over 60s can hugely benefit from eating extra protein:
1.0 - 1.3 g/kg of body weight

The UK RDA for protein is 0.75g / kg of bodyweight. However "These recommendations are derived as a minimum amount to maintain nitrogen balance and are not optimised for physical activity level (PAL). Individuals with low physical activity levels have decreased rates of nitrogen retention and therefore in order to maintain muscle tissue have increased protein requirements in comparison to those who are active. Considering that physical activity decreases with age, this is an important factor when protein needs are evaluated. Furthermore, the body of an ageing adult undergoes multiple physiological changes which alter protein utilisation, and thus requirements".
Ref: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872778/
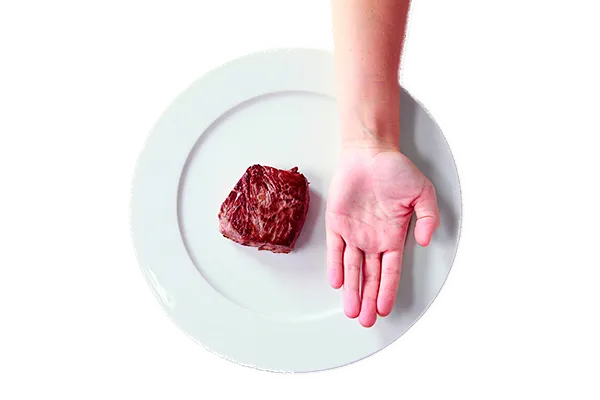
What would this look like in practice?
1.3 g/kg of protein would equate to a palm to a plam and a half sized portion of protein in 3 meals across the day for a 70kg person.
Meat
Fish
Eggs
Dairy
SUPPLEMENTATION OF CREATINE
